Understanding OCD: A Neuroimaging Perspective
Obsessive-Compulsive Disorder (OCD) is a mental health condition characterised by persistent, intrusive thoughts (obsessions) and repetitive behaviours or mental acts (compulsions) that an individual feels driven to perform to alleviate the anxiety caused by the obsessions. These obsessions and compulsions can significantly interfere with daily functioning and quality of life.
OCD is a complex disorder with a range of manifestations, including:
- Contamination obsessions and cleaning compulsions
- Checking compulsions (e.g., repeatedly checking locks, appliances, or personal safety)
- Symmetry obsessions and ordering/arranging compulsions
- Intrusive thoughts about harm or violence
- Hoarding behaviours
The symptoms of OCD can vary widely in severity, from mild to debilitating, and can fluctuate over time. While the exact cause of OCD is not fully understood, research suggests that a combination of genetic, neurobiological, and environmental factors contribute to its development.
Causes and risk factors of OCD
OCD is a multifactorial disorder, with various factors contributing to its development and manifestation. Here are some key causes and risk factors:
- Genetic factors: OCD has a strong genetic component, with studies indicating that individuals with a first-degree relative with OCD are at a higher risk of developing the disorder.
- Brain chemistry: Imbalances in neurotransmitters, such as serotonin, dopamine, and glutamate, have been implicated in the development of OCD symptoms.
- Environmental factors: Stressful life events, traumatic experiences, and certain infections or illnesses have been associated with the onset or exacerbation of OCD symptoms.
- Neurological factors: Structural and functional abnormalities in specific brain regions, including the orbitofrontal cortex, anterior cingulate cortex, and striatum, have been linked to OCD.
- Age and gender: OCD can develop at any age, but the onset is most common in childhood, adolescence, and early adulthood. The disorder affects both males and females, although some research suggests a slightly higher prevalence in females.
It’s important to note that the causes and risk factors of OCD are complex and can vary from individual to individual. A comprehensive understanding of these factors is crucial for developing effective treatment strategies.
Understanding the brain and OCD: An overview of neuroimaging
Neuroimaging techniques have revolutionised our understanding of the brain and its role in various mental health conditions, including OCD. These techniques allow researchers to visualise and study the structure and function of the brain, providing valuable insights into the neurobiological mechanisms underlying OCD.
Neuroimaging has played a pivotal role in elucidating the brain regions and neural networks involved in OCD, as well as the functional and structural abnormalities associated with the disorder. By examining the brain in action, neuroimaging studies have shed light on the complex interplay between cognition, emotion, and behaviour in individuals with OCD.
Neuroimaging techniques used in studying OCD – FMRI, PET, and MRI
Several neuroimaging methods have been employed in the study of OCD, each offering unique insights into the brain’s structure and function. Here are some of the most commonly used techniques:
- Functional Magnetic Resonance Imaging (fMRI): fMRI measures changes in blood oxygenation levels in the brain, which are closely related to neural activity. This technique allows researchers to observe which brain regions are activated or deactivated during specific tasks or stimuli, providing valuable information about the neural correlates of OCD symptoms and cognitive processes.
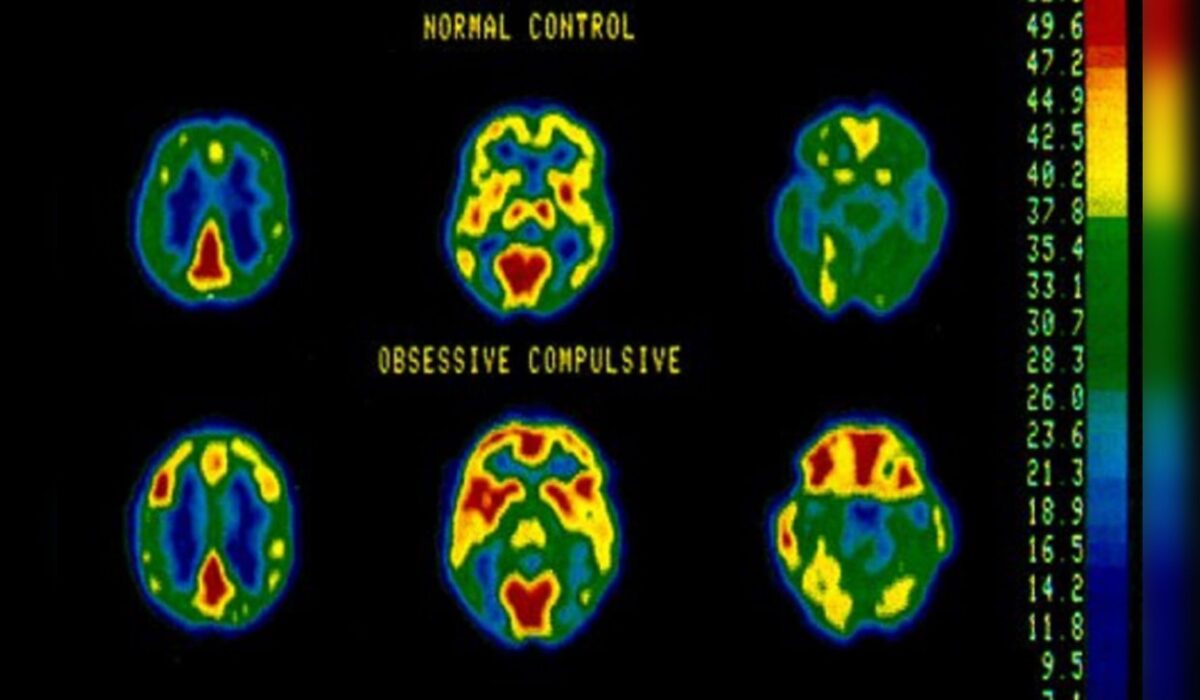
- Positron Emission Tomography (PET): PET scans use radioactive tracers to measure various aspects of brain function, such as glucose metabolism, neurotransmitter activity, and receptor binding. PET studies have been instrumental in understanding the role of neurotransmitter systems, particularly serotonin and dopamine, in OCD.
- Structural Magnetic Resonance Imaging (sMRI): sMRI provides detailed images of the brain’s anatomy and structure, allowing researchers to examine potential structural abnormalities or differences in brain regions associated with OCD. This technique has been used to investigate the grey matter and white matter abnormalities in individuals with OCD.
These neuroimaging techniques have been used in conjunction with various experimental paradigms, such as symptom provocation, cognitive tasks, and treatment response studies, to gain a comprehensive understanding of the neural mechanisms underlying OCD.
Neuroimaging findings in OCD: Key insights into the brain mechanisms
Neuroimaging studies have yielded valuable insights into the brain mechanisms involved in OCD, shedding light on the neural circuits and regions that play a crucial role in the development and maintenance of the disorder. Here are some key neuroimaging findings in OCD:
- Cortico-striato-thalamo-cortical (CSTC) circuit abnormalities: The CSTC circuit, which includes the orbitofrontal cortex, anterior cingulate cortex, striatum, and thalamus, has been consistently implicated in OCD. Functional and structural abnormalities in this circuit have been associated with the obsessions, compulsions, and cognitive inflexibility observed in individuals with OCD.
- Hyperactivation of the orbitofrontal cortex and anterior cingulate cortex: Neuroimaging studies have consistently shown increased activation in the orbitofrontal cortex and anterior cingulate cortex during symptom provocation or cognitive tasks in individuals with OCD. These regions are involved in decision-making, emotional processing, and conflict monitoring, which may contribute to the persistent and intrusive thoughts and behaviours characteristic of OCD.
- Abnormalities in the striatum and thalamus: The striatum and thalamus, which are part of the CSTC circuit, have also been implicated in OCD. Functional and structural abnormalities in these regions have been associated with the repetitive behaviours and cognitive inflexibility observed in individuals with OCD.
- Altered connectivity and network dysfunction: Recent neuroimaging studies have focused on examining the functional and structural connectivity between different brain regions in OCD. Findings suggest that altered connectivity and network dysfunction, particularly within the CSTC circuit and between limbic and cognitive control regions, may contribute to the development and maintenance of OCD symptoms.
- Neurotransmitter system abnormalities: Neuroimaging studies using PET have revealed abnormalities in neurotransmitter systems, particularly the serotonin and dopamine systems, in individuals with OCD. These findings have contributed to developing pharmacological treatments targeting these neurotransmitter systems.
It’s important to note that while these neuroimaging findings have provided valuable insights, OCD is a heterogeneous disorder, and individual differences in brain structure and function may contribute to the diverse symptom presentations and treatment responses observed in individuals with OCD.
The role of neuroimaging in the diagnosis and treatment of OCD
Neuroimaging has played a crucial role in advancing our understanding of OCD and has the potential to inform both the diagnosis and treatment of the disorder. Here are some ways in which neuroimaging can contribute to the management of OCD:
- Diagnostic biomarkers: While neuroimaging is not currently used as a diagnostic tool for OCD, ongoing research aims to identify potential neuroimaging biomarkers that could aid in the early and accurate diagnosis of the disorder. These biomarkers could include structural or functional abnormalities in specific brain regions or networks associated with OCD.
- Treatment planning and monitoring: Neuroimaging can provide valuable insights into the neural mechanisms underlying treatment response in OCD. By examining changes in brain activity or connectivity before and after treatment, neuroimaging can help identify potential predictors of treatment response and guide the selection of appropriate interventions.
- Monitoring treatment efficacy: Neuroimaging can be used to monitor the effects of various treatments, such as cognitive-behavioral therapy (CBT) or pharmacological interventions, on brain function and structure. This can help researchers and clinicians evaluate the efficacy of different treatment approaches and potentially optimise treatment strategies for individual patients.
- Neurofeedback and brain stimulation techniques: Neuroimaging findings have paved the way for developing novel treatment approaches, such as neurofeedback and brain stimulation techniques like transcranial magnetic stimulation (TMS) or deep brain stimulation (DBS). These techniques aim to modulate brain activity in specific regions or networks implicated in OCD, potentially providing alternative treatment options for individuals who do not respond to traditional therapies.
- Personalised medicine: By combining neuroimaging data with genetic, clinical, and behavioural information, researchers hope to develop personalised treatment approaches tailored to the specific neurobiological profile of each individual with OCD. This could lead to more effective and targeted interventions, improving treatment outcomes and quality of life for those affected by the disorder.
While neuroimaging has made significant contributions to our understanding of OCD, it is essential to note that these techniques should be used in conjunction with comprehensive clinical assessments and evidence-based treatment approaches.
Limitations and challenges of neuroimaging in OCD research
Despite the valuable insights provided by neuroimaging studies, there are several limitations and challenges associated with the use of these techniques in OCD research:
- Heterogeneity of OCD: OCD is a highly heterogeneous disorder with diverse symptom presentations and potential subtypes. This heterogeneity can make it challenging to identify consistent neuroimaging findings across different studies and populations.
- Small sample sizes: Many neuroimaging studies in OCD have relatively small sample sizes, which can limit the statistical power and generalizability of the findings.
- Comorbidities and medication effects: OCD often co-occurs with other mental health conditions, and individuals with OCD may be taking various medications. These factors can potentially confound neuroimaging findings and make it difficult to disentangle the specific effects of OCD from those of comorbidities or medications.
- Reverse inference limitations: While neuroimaging can identify brain regions or networks associated with OCD, it is crucial to recognise the limitations of reverse inference. Activation or abnormalities in specific brain regions do not necessarily imply a direct causal relationship with OCD symptoms or behaviours.
- Temporal resolution limitations: Most neuroimaging techniques have limited temporal resolution, making it challenging to capture the rapid dynamics of brain activity associated with specific cognitive or behavioural processes in OCD.
- Ecological validity concerns: Neuroimaging studies often involve highly controlled experimental settings, which may not fully capture the complexity of real-world situations and experiences encountered by individuals with OCD.
- Ethical and practical considerations: Neuroimaging research can be expensive and time-consuming and may involve potential risks or discomfort for participants. Ethical considerations, such as informed consent and data privacy, must also be carefully addressed.
Researchers employ various strategies to address these limitations and challenges, such as multimodal neuroimaging approaches, larger sample sizes, careful control for confounding factors, and integrating neuroimaging data with other behavioural, genetic, and clinical measures.
Future directions in neuroimaging research for OCD
As neuroimaging techniques continue to advance and our understanding of OCD deepens, several exciting future directions in neuroimaging research for OCD are emerging:
- Multimodal neuroimaging approaches: Combining multiple neuroimaging techniques, such as fMRI, PET, and sMRI, can provide a more comprehensive understanding of the structural, functional, and neurochemical abnormalities associated with OCD. This multimodal approach may help unravel the complex interplay between different brain systems and mechanisms underlying the disorder.
- Longitudinal and developmental studies: Longitudinal neuroimaging studies that follow individuals with OCD over time can provide valuable insights into the trajectory of brain changes associated with the disorder and the potential impact of interventions. Additionally, developmental neuroimaging studies can shed light on the neural mechanisms underlying the onset and progression of OCD in childhood and adolescence.
- Neuroimaging-guided interventions: As our understanding of the neural correlates of OCD deepens, neuroimaging data may be used to guide and optimise personalised treatment approaches. For example, neurofeedback or brain stimulation techniques could be tailored to target specific brain regions or networks implicated in an individual’s OCD symptoms.
- Machine learning and artificial intelligence: Integrating machine learning and artificial intelligence techniques with neuroimaging data holds promise for developing predictive models and identifying biomarkers for OCD. These approaches may aid in early diagnosis, treatment selection, and monitoring of treatment response.
- Connectivity and network analyses: Advances in functional and structural connectivity analyses and graph theory approaches can provide valuable insights into complex brain networks and their interactions in OCD. This may help elucidate the neural mechanisms underlying the cognitive, affective, and behavioural aspects of the disorder.
- Integration with other ‘omics’ data: Combining neuroimaging data with other ‘omics’ data, such as genomics, proteomics, and metabolomics, can provide a more comprehensive understanding of the biological mechanisms underlying OCD. This integrative approach may lead to identifying novel biomarkers and targets for intervention.
- Virtual reality and ecological neuroimaging: Integrating virtual reality and ecological neuroimaging techniques can enhance the ecological validity of neuroimaging studies by simulating real-world scenarios and environments relevant to OCD. This may provide a more accurate representation of the neural processes involved in the disorder.
As neuroimaging research in OCD continues to evolve, it is essential to foster interdisciplinary collaborations, address ethical considerations, and ensure the translation of research findings into clinical practice to improve the lives of individuals affected by this debilitating disorder.
How neuroimaging can inform treatment approaches for OCD
Neuroimaging has the potential to significantly inform and guide the development of more effective treatment approaches for OCD. By providing insights into the neural mechanisms underlying the disorder, neuroimaging findings can contribute to the refinement and optimisation of existing treatments and the exploration of novel interventions. Here are some ways in which neuroimaging can inform treatment approaches for OCD:
- Identifying treatment targets: Neuroimaging studies have identified specific brain regions and networks that are dysregulated in OCD, such as the cortico-striato-thalamo-cortical (CSTC) circuit, orbitofrontal cortex, and anterior cingulate cortex. These regions can serve as potential targets for interventions like cognitive-behavioural therapy (CBT), neurofeedback, or brain stimulation techniques like transcranial magnetic stimulation (TMS) or deep brain stimulation (DBS).
- Predicting treatment response: Neuroimaging data can be used to identify potential biomarkers or neural signatures that predict an individual’s response to specific treatments. For example, researchers have found that baseline activity or connectivity patterns in specific brain regions may be associated with better or worse treatment outcomes for CBT or pharmacotherapy. This information can help clinicians personalise treatment plans and optimise the selection of interventions for each individual.
- Monitoring treatment efficacy: Neuroimaging can monitor changes in brain activity or connectivity before and after treatment, providing objective measures of treatment efficacy. This can help clinicians evaluate the effectiveness of interventions and make informed decisions about continuing, modifying, or changing treatment approaches.
- Developing novel interventions: Neuroimaging findings have paved the way for the development of novel treatment approaches that directly target the neural mechanisms underlying OCD. For example, neurofeedback and brain stimulation techniques like TMS or DBS aim to modulate activity in specific brain regions or networks implicated in OCD, potentially providing alternative treatment options for individuals who do not respond to traditional therapies.
- Enhancing existing treatments: Neuroimaging data can inform the refinement and optimisation of existing treatments like CBT or exposure and response prevention (ERP) therapy. By understanding the neural correlates of symptom provocation, cognitive processes, and treatment response, clinicians can tailor and enhance these interventions to target specific neural mechanisms more effectively.
- Multimodal treatment approaches: Neuroimaging findings can guide the development of multimodal treatment approaches that combine pharmacological interventions, psychotherapy, and brain stimulation techniques. By targeting different aspects of the neural mechanisms underlying OCD, these multimodal approaches may lead to more comprehensive and effective treatment outcomes.
- Personalised medicine: Integrating neuroimaging data with other clinical, genetic, and behavioural information can contribute to developing personalised medicine approaches for OCD. By understanding an individual’s unique neurobiological profile, clinicians can tailor treatment strategies to their specific needs, potentially improving treatment outcomes and quality of life.
It is important to note that while neuroimaging holds great promise for informing treatment approaches, it should be used in conjunction with comprehensive clinical assessments and evidence-based practices. Ongoing research and interdisciplinary collaborations are crucial to translating neuroimaging findings into clinical applications that can benefit individuals with OCD.
Conclusion: The importance of neuroimaging in unravelling the complexities of OCD
Obsessive-Compulsive Disorder (OCD) is a complex and debilitating mental health condition that affects millions of individuals worldwide. Neuroimaging techniques have revolutionised our understanding of the brain mechanisms underlying OCD, providing valuable insights into the structural, functional, and neurochemical abnormalities associated with the disorder.
Through techniques like functional magnetic resonance imaging (fMRI), positron emission tomography ( PET), and structural MRI, researchers have identified key brain regions and networks implicated in OCD, such as the cortico-striato-thalamo-cortical (CSTC) circuit, orbitofrontal cortex, anterior cingulate cortex, and abnormalities in neurotransmitter systems like serotonin and dopamine. These findings have not only deepened our understanding of the neural underpinnings of OCD but have also paved the way for developing novel treatment approaches and optimising existing interventions.
Neuroimaging has the potential to inform various aspects of OCD management, from diagnosis and treatment planning to monitoring treatment efficacy and developing personalised medicine approaches. By identifying potential biomarkers or neural signatures associated with treatment response, neuroimaging data can guide the selection of appropriate interventions and help clinicians tailor treatment plans to individual needs. Moreover, novel interventions like neurofeedback and brain stimulation techniques aim to directly modulate activity in specific brain regions or networks implicated in OCD, offering alternative treatment options for those who do not respond to traditional therapies.
Despite neuroimaging’s valuable contributions, some limitations and challenges must be addressed, such as OCD’s heterogeneity, small sample sizes, comorbidities, and ecological validity concerns. Ongoing research efforts are focusing on multimodal neuroimaging approaches, longitudinal and developmental studies, machine learning and artificial intelligence integration, and exploring connectivity and network analyses to gain a more comprehensive understanding of the neural mechanisms underlying OCD.
As we continue to unravel the complexities of OCD through neuroimaging research, it is crucial to foster interdisciplinary collaborations, address ethical considerations, and ensure the translation of research findings into clinical practice. Combining neuroimaging insights with other ‘omics’ data, clinical assessments, and evidence-based practices can pave the way for more effective and personalised treatment approaches, ultimately improving the quality of life for individuals affected by this debilitating disorder.
If you or someone you know is struggling with OCD, it is essential to seek professional help. Consider reaching out to a mental health professional or support group for guidance and support on your journey to recovery. Remember, with the proper treatment and support, it is possible to manage and overcome the challenges of OCD.